Mary Potter/ Photos by Ivan Potter
Sunday, July 10, 2011 8:19 pm
|
(Paducah, KY, July 8, 2011) - Governor Beshear and Cabinet for Health and Human Services Secretary Janie Miller flew into Paducah on Friday in a fly around to sell the public on a new improved management program for Medicaid.
Medicaid is the program that provides medical services to children through KCHIP (Kentucky Children’s Insurance Program), lower income women, the disabled and patients needing long term care. Medicaid Program webpage The program is funded with both state and federal funds – but is managed by the state.
The program now serves 815,000 Kentuckians, the largest number of recipients since it began in 1965. And it’s proved to be a budget buster. With the worsening national economy, more people apply for and are eligible for services. At the same time, health care costs have skyrocketed.
Funding problems came to a head when Congress failed to allocate $100 million dollars to the program. States looking to use federal money, like Kentucky, were thrown into disarray
Putting management of Medicaid in the hands of private providers is his answer. A system of “managed care” across the state will go into effect as of October 1st. Around 560,000 Kentucky recipients will be affected by the change. Kentucky is not the first to go this route. Over half the states have managed Medicaid programs.
Managed care is not new to Medicaid in Kentucky. Passport Health Plan is in place in Region 3- Jefferson County and twelve surrounding counties. Passport manages care for 170,000 patients. Passport Health made news in the recent past when an investigation found profligate spending by company executives.
Beshear said the offenders are gone. He said his administration had worked with Auditor Crit Luallen and the company to put new controls in place. Beshear said that the complaints were not about the care provided by Passport Health. The controls in place for Passport will be applied to the three new companies that will compete for every region, except the one covered by Passport Health.
All three of the new providers: Coventry Cares of Kentucky, a Medicaid product of Coventry Health and Life Insurance Company of Delaware, WellCare of Kentucky, a part of WellCare health Insurance of Illinois and Kentucky Spirit Health Plan, a subsidiary of Centene Corporation headquartered in Missouri, will compete for the same customer base in the same territory. Competition, it is hoped, will lead to better services. Payments will be made on a per patient basis and will be made monthly. The idea is that the better companies will attract more customers, increasing their share of the pot. More efficient companies will be able to keep more of the dollars they earn.
They will be required to have offices in Kentucky. They are projected to add 550 jobs in the state. The Governor was asked if any of the jobs would be in West Kentucky. He didn’t know where the new jobs would go – just that they would be Kentucky jobs. When asked if her Cabinet would shed jobs because of the new program, Secretary Miller did not think it would. Employees with expertise in Medicaid will be needed to oversee the new programs.
The Governor compared managed care for Medicaid to insurance choices offered to employees with access to more than one plan (like government employees). The plans were offer different programs to attract patients. Cabinet Secretary Miller said some have wellness programs that provide incentives to those who work to prevent chronic disease, like diabetes. Secretary Miller spoke of small incentives to those in the program to fight childhood obesity and make healthy lifestyle choices.
Choo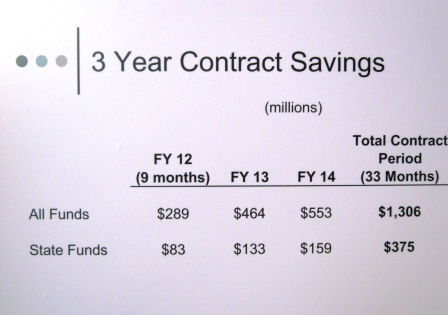
The Governor predicts that the state will save $1.3 billion dollars in Medicaid funds and $375 million in General funds during the initial 33 month contracts. (See Chart at left).
Governor Beshear said that he expects there to be “bumps in the road” in the implementation of the new program. But he does not expect recipients to see a change in the health services they receive.
